2019-04-12
作者:广东省肺癌研究所 杨学宁 & LAMP
272. Surgical Resection and Perioperative Chemotherapy for N1 Positive Stage II Non-Small Cell Lung Cancer (NSCLC): Better Than Expected Outcomes Particularly in Patients with Solitary Nodal Metastasis
Abby White1, Suden Kucukak1, Daniel N. Lee1, *Raphael Bueno1, *Yolonda L. Colson1, *Michael T. Jaklitsch1, *Steven J. Mentzer1, Jon O. Wee1, *David J. Sugarbaker2, *Scott J. Swanson1
1Brigham & Women's Hospital, Boston, MA;2Baylor College of Medicine, Houston, TX
Objective: Surgical resection and perioperative chemotherapy for N1 positive stage II non-small cell lung cancer (NSCLC): Better than expected outcomes particularly in patients with solitary nodal metastasis. Stage II NSCLC represents a minority distribution (~8%) of the approximately 234,000 diagnosed cases per year. Survival ranges from 53-60%. Randomized controlled trials have demonstrated a modest 5.4% survival benefit with adjuvant chemotherapy, but have included heterogenous patient populations and stage distributions. Large database analyses have questioned the role of perioperative chemotherapy in resected stage II patients, but without much granular detail regarding staging, surgery and chemotherapy. This single-institution study sought to evaluate the outcomes of surgical resection for Stage II, N1(+) NSCLC and the effect of perioperative chemotherapy.
Methods: All patients with resected stage II, N1-positive NSCLC between 2010 and 2016 were included in this study. A retrospective chart review was conducted and comprehensive clinicopathologic data were collected relative to staging, surgery, pathologic review, and perioperative oncology treatment.
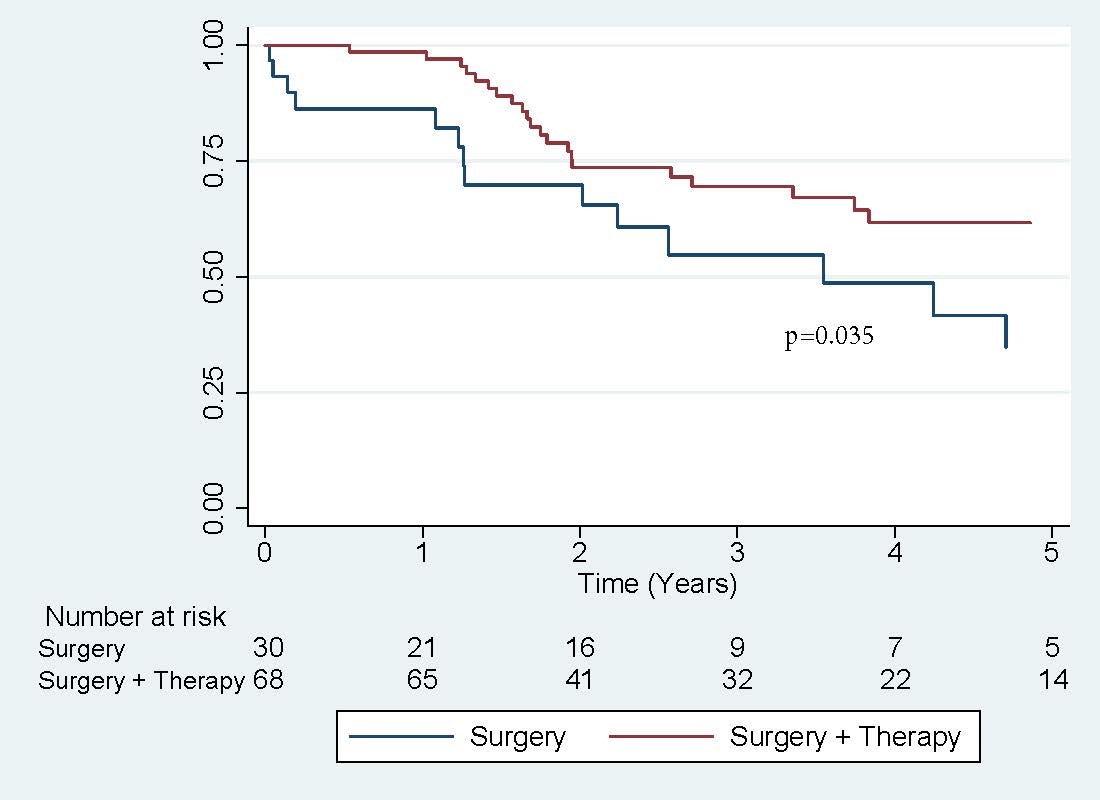
Results: Ninety patients with surgically-resected stage II, N1-positive disease were identified for analysis, which included 44 males with median age 69. Seventy-six patients underwent lobectomy (77.6%), 63 by VATS (64.3%) Fifty-three patients (54.1%) had a solitary N1, metastasis and 45 patients (45.9%) had multiple N1 nodal metastases. Five-year OS (66.4% vs 38.5%, p=0.015) and disease-free survival (57.7% vs. 18.7%, p=0.00) were significantly higher in patients with solitary N1 metastasis. Sixty-five percent (64/98) of all N1-positive patients received adjuvant chemotherapy, and their survival was significantly better than those who underwent surgery alone (61.7% vs 34.8%, p = 0.035). Forty-seven (73.4%) patients completed 4 cycles of chemotherapy. Median time to initiation of adjuvant chemotherapy was 53 days, with a range of 22-269 days. Timing of adjuvant therapy (>or<60 days) did not have significant impact on 5-year OS or DFS. Ten patients (10.2%) received neoadjuvant therapy, with no difference in OS or DFS compared to the rest of the cohort.
Conclusions: Patients who had surgical resection and perioperative chemotherapy for N1 positive NSCLC had favorable survival at 5 years and those with solitary N1 lymph node metastasis had survival comparable to stage I NSCLC. The magnitude of chemotherapy benefit (27% in this study) may be under-estimated by available literature. Timing of adjuvant therapy does not appear to have significant impact on survival.
推荐阅读
文章评论
注册或登后即可发表评论
登录/注册
全部评论(0)