2019-04-12
作者:广东省肺癌研究所 杨学宁 & LAMP
257. What Really Happens at 30 and 90 Days After Pneumonectomy?
Gregory David Jones, Raul Caso, Kay See Tan, Joseph Dycoco, *Bernard J. Park, Matthew Bott, *Daniela Molena, *James Huang, James Isbell, *David R. Jones, *Gaetano Rocco
Memorial Sloan Kettering Cancer Center, New York, NY
Invited Discussant: *Thomas A. D’Amico
Objective: Pneumonectomy has the highest mortality rate among lung cancer operations, with 30-day rates in the 5-10% range. With recent focus on streamlined post-operative care, regimented follow-up, and systematic reporting of complications, a deeper analysis into readmissions, complications, and deaths at specific time points is warranted. This study aims to examine 30-day readmission and 90-day mortality rates and to identify potential factors associated with these outcomes.
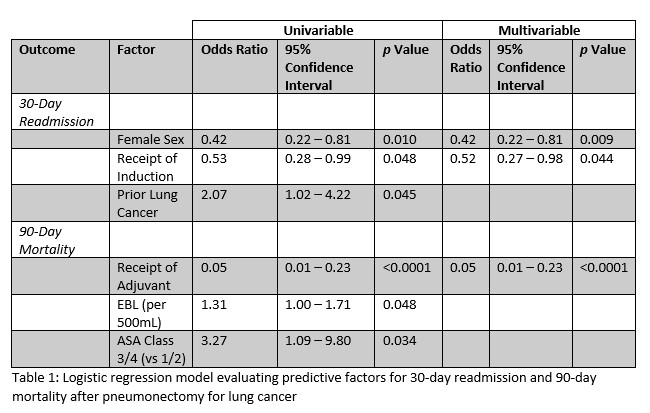
Methods: A retrospective review of a prospectively maintained database was conducted for all pneumonectomies performed for lung cancer at single institution from 2000 to 2018. In-hospital complications and mortality, as well as complications, readmissions, and mortality at 30- and 90-days post-surgery were reported using Clavien-Dindo classification. Logistic regression analysis was used to determine factors associated with 30-day readmission and 90-day mortality, using odds ratios (ORs) and 95% confidence intervals (CIs). Disease-free and overall survival (DFS, OS) were estimated using Kaplan-Meier approach.
Results: A total of 355 pneumonectomies were performed for lung cancer from 2000-2018. The median length of stay was 6 days (range, 0-69), with 123 (34%) patients experiencing an in-hospital complication of any grade. By 30-days post-surgery, 47 (13%) patients were readmitted, and 16 (4.5%) died, including 13 (3.7%) in-hospital deaths. From 31-90 days, an additional 32 (9.4%) patients were readmitted, and a total of 24 (6.8%) patients died by 90 days. Logistic regression showed that female gender (OR 0.42, 95% CI 0.22-0.81, p=0.010) and receipt of induction therapy (OR 0.53, 95% CI 0.28-0.99, p=0.048) were associated with lower odds of 30-day readmission, whereas history of prior lung cancer (OR 2.07, 95% CI 1.02-4.22, p=0.045) was associated with higher odds of 30-day readmission. At 90 days, ASA class of 3/4 (vs. 1/2, OR 3.27, 95% CI 1.09-9.80, p=0.034) and higher EBL (OR 1.31 per 500mL, 95% CI 1.00-1.71, p=0.048) were associated with higher mortality, while receipt of adjuvant therapy was associated with lower mortality (OR 0.05, 95% CI 0.01-0.23, p<0.0001). Five-year DFS and OS for all pathologic stages were 33.3% (95% CI 28.0-38.6%) and 40.8% (95% CI 35.1-46.5%), respectively.
Conclusions: This temporal analysis of factors associated with readmissions, complications, and deaths up to 90 days after surgery shows that more than half (54%) of patients who experienced 90-day mortality died during the initial hospitalization. Only an additional 2.3% of patients died between 30 and 90 days, suggesting that the “hidden mortality” at 90 days previously proposed in the literature may be overstated. This also prompts a thorough investigation into the factors associated with improved peri- and post-operative morbidity and mortality for this high-risk surgical procedure.
推荐阅读
文章评论
注册或登后即可发表评论
登录/注册
全部评论(0)