2019-04-12
194. Short and Long-Term Outcomes Following Surgery for Primary Mediastinal Nonseminomatous Germ Cell Tumors in the Cisplatin Era
*Kenneth A. Kesler, Amanda R. Stram, Lava R. Timsina, *Mark W. Turrentine, *John W. Brown, Lawrence H. Einhorn
Indiana University, Indianapolis, IN
Invited Discussant: *John A. Howington
Objective: Primary mediastinal nonseminomatous germ cell tumors (PMNSGCT) represent a rare but important malignancy originating in the anterior mediastinum in otherwise young and healthy patients. Treatment is challenging and involves cisplatin-based chemotherapy followed by surgery to remove residual disease. The goal of this study was to further define outcomes with a 10-year update of our previously published 2008 institutional experience.
Methods: We performed a retrospective study of all patients who underwent surgical resection of PMNSGCT following chemotherapy at our institution from 1982 to 2017.
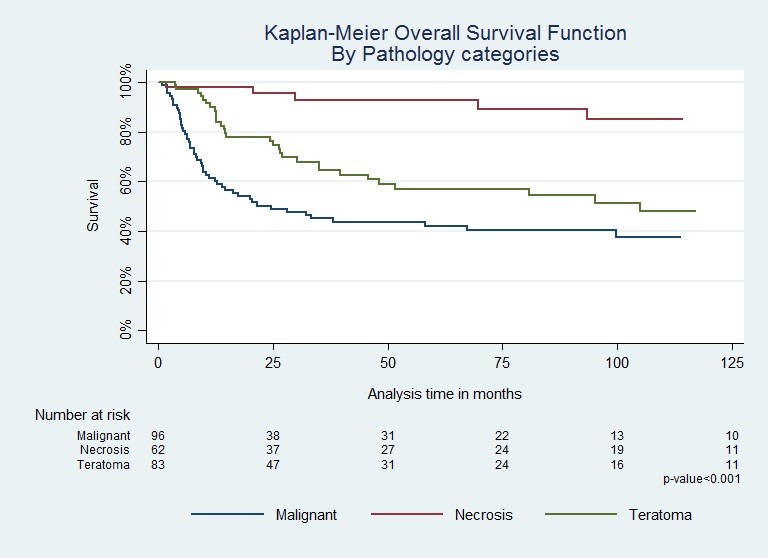
Results: A total of 252 patients (age = 29.2 ± 8.4 yrs) were identified. 225 (95.7%) patients had elevated serum tumor markers (alphafetoprotein or β-human chorionic gonadotropin) at the time of diagnosis. 78 (34.2%) patients presented with metastatic disease and 38 with extrathoracic metastases. 160 (66.4%) patients received bleomycin-containing combination chemotherapy prior to surgery. Overall, there were 11 (4.4%) postoperative deaths.Acute respiratory distress syndrome (ARDS) occurred postoperatively in 27 (10.7%) patients, which was responsible for 10 of these deaths equating to a 37.0% mortality of ARDS. Of patients who developed ARDS, significantly more patients received bleomycin-containing chemotherapy (n=25, 92.6% vs. n=2, 7.4%, p=0.004).With respect to long-term survival, normal tumor markers at time of surgery was protective (n=149, 61.8%) (HR=0.05, p=0.001). Conversely, rising markers (n=44, 18.3%) and elevated AFP (n=83, 34.4%) at surgery were independent predictors of death (HR=2.01, p=0.006 and HR=1.96, p=0.002, respectively). We confirmed our previous findings that the “worst” pathology identified in the residual mass significantly impacted overall survival: complete necrosis in 62 (25.7%), teratoma (with or without stromal atypia) in 83 (34.4%), and malignant (persistent germ cell or non-germ cell cancer) in 96 (39.8%) (p<0.001, Figure 1). Additionally however, teratoma with stromal atypia (n=18) demonstrated decreased overall survival compared to teratoma without atypia (n=65, p=0.037), and patients with malignancy involving >50% of the residual mass (n=47) had a 2.3-fold increased risk of death compared to patients with malignancy involving ≤50% (n=44, p=0.009).
Conclusions: Our large institutional experience demonstrates preoperative serum tumor markers and postchemotherapy pathology categories as independent predictors of long-term survival. Within the teratoma and malignant histology categories, the presence or absence of stromal atypia, and residual masses containing > or ≤ 50% cancer were also significant variables, respectively. Avoiding bleomycin-containing chemotherapy prior to major thoracic surgical procedures remains important to minimize postoperative respiratory complications and related mortality.
推荐阅读
文章评论
注册或登后即可发表评论
登录/注册
全部评论(0)