2019-04-12
作者:广东省肺癌研究所 杨学宁 & LAMP
270. Surgery in Large Cell Lung Neuroendocrine Cancer: A National Analysis
Vignesh Raman1, Oliver K. Jawitz1, Paul J. Speicher1, Chi-Fu J. Yang2, *Betty C. Tong1, Jacob Klapper1, *Matthew G. Hartwig1, *Thomas A. D'Amico1, *David H. Harpole1
1Duke University, Durham, NC;2Stanford University, Palo Alto, CA
Objective: Compared to other histologic subtypes of non-small cell lung cancer, large cell neuroendocrine cancer (LCNEC) portends a poor prognosis. There is increasing recognition that LCNEC behaves similarly to small cell lung cancer (SCLC), which may make it less amenable to surgery. We investigated the benefit of surgery compared to definitive therapy in LCNEC.
Methods: Patients with cT1-3N0-2M0 LCNEC were identified in the National Cancer Database (2004-2015). Exclusion criteria included incomplete treatment or staging information and incomplete definitive therapy. Patients were grouped by type of treatment: no therapy, definitive chemoradiation, or surgery with or without appropriate perioperative therapy. Both wedge and segmental resections were categorized as sublobar. Overall survival was analyzed with Kaplan-Meier and Cox proportional hazards models.
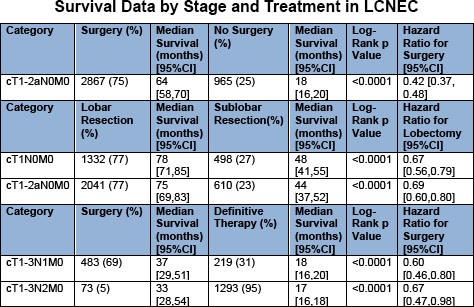
Results: Of 39,187 patients with LCNEC, 11,380 (29%) underwent surgery. Lobectomy (64%) and wedge resection (16%) were the most commonly performed operations. Of 3832 patients with clinical stage I disease, 2867 (75%) underwent surgery (Table 1). Surgery was associated with a significant increase in survival (hazard ratio [HR]0.42; 95% confidence interval [CI]0.37, 0.48) compared to no surgery. A total of 2041 (77%) patients with stage I disease underwent lobectomy while 610 (23%) underwent sublobar resection. Lobectomy was associated with a survival benefit compared to sublobar resection (HR 0.69; 95%CI 0.60,0.80) in both stage I overall and in the stage IA subgroup (HR 0.67; 95%CI 0.56,0.79). Of 702 patients with cT1-3N1M0 disease, 483 (69%) underwent surgery, while 219 (31%) received definitive therapy. Compared to definitive chemoradiation, surgery was associated with a survival benefit (HR 0.60; 95%CI 0.46,0.80) in N1 disease. Only 226 (53%) of 426 patients who underwent surgery for N1 disease received adjuvant therapy, which was associated with improved survival compared to no adjuvant therapy (HR 0.68; 95%CI 0.48,0.96). Comparatively, only 73 (5%) patients underwent surgery following induction therapy for cT1-3N2M0 LCNEC, where surgery again independently predicted survival compared to definitive therapy (HR 0.67; 95%CI 0.47, 0.98). When surgery (n=629; 32%) with or without perioperative therapy was compared to definitive therapy (n=1346) in N2 disease, surgery remained an independent predictor of survival (HR 0.73; 95%CI 0.63,0.85).
Conclusions: Surgery is associated with a significant survival benefit compared to definitive chemoradiation in patients with both early and regionally advanced LCNEC. Lobectomy is associated with improved survival compared to sublobar resection in early LCNEC. Lobectomy should be considered for patients with resectable T1-3N0-2M0 LCNEC who are medically fit.
Lobectomy Is Superior to Sublobar Resection for Stage I Large Cell Neuroendocrine Carcinoma of the Lung
对于I期肺大细胞神经内分泌癌患者,肺叶切除术优于亚肺叶切除
*Niv Ad1, Sari D. Holmes2, *Bradley S. Taylor3, Stefano Schena4, Diane Alejo4, Clifford E. Fonner5, Rawn Salenger6, *Glenn J. R. Whitman4, Thomas S. Metkus, Jr4, Chetan Pasrija3, Mehrdad Ghoreishi3, Paul S. Massimiano1, Anthony J. Rongione1
作者单位:1Washington Adventist Hospital, Takoma Park, MD; 2WVU Heart and Vascular Institute, Morgantown, WV; 3University of Maryland Heart & Vascular Center, Baltimore, MD; 4The Johns Hopkins University, Baltimore, MD; 5Maryland Cardiac Surgery Quality Initiative, Baltimore, MD; 6University of Maryland School of Medicine, Towson, MD
讨论嘉宾:*M. Blair Marshall
目的
目前,使用亚肺叶切除手术方式来处理早期肺癌有增多的趋势。在特定的患者中,接受亚肺叶切除患者的生存率与接受肺叶切除术患者的生存率相当。然而,对于诸如肺大细胞神经内分泌癌(LCNEC)等不常见的肺癌病理类型,手术切除范围对患者生存率的影响尚不清楚。在这里,我们使用一个国家数据库的临床数据来比较I期LCNEC患者在接受肺叶切除术或亚肺叶切除术后的预后情况。
方法
利用监测、流行病学和最终结果(SEER)数据库,筛选出1988年至2012年所有经手术切除的I期LCNEC病例。根据AJCC第8版的定义重新进行癌症分期。同时对以下变量(年龄、性别、种族、肿瘤位置、分期、病理分级和手术类型)进行核查。采用Kaplan-Meier方法和多变量Cox比例风险模型评估生存率并筛选独立预后因子。
结果
共407例纳入分析。大多数患者(n=316,77.6%)接受了肺叶切除术。单变量分析显示,亚肺叶切除术与高龄(P<0.001)和早期(IA与IB,P=0.01)显著相关。所有I期LCNEC患者1年、3年和5年总生存率,肺叶切除术后分别为89.5%、72.7%和63%,而亚肺叶切除术后分别为84%、56%和41%(P=0.004)。当按分期进行分层分析时:IA期(肺叶切除术:92%、79.2%和66%,亚肺叶切除术:87%、54.1%和45%;P=0.009),IB期(肺叶切除术:86.5%、63.4%和59.2%,亚肺叶切除术:76%、59.4%和33.5%;P=0.079),结果显示接受肺叶切除术的患者1年、3年和5年总生存率更佳。当按年龄进行分层分析时,70岁以下的患者(肺叶切除术:92%、78%和68%,亚肺叶切除术:89%、58%和42.5%;P=0.027)显示了相似的结果,但70岁以上的患者(P=0.299)无类似趋势。在多变量Cox比例风险分析中,高龄(HR 1.051,P<0.001)、IB期(HR 1.48,P=0.023)和亚肺叶切除术(HR 1.64,P=0.008)因素与死亡风险增加显著相关。
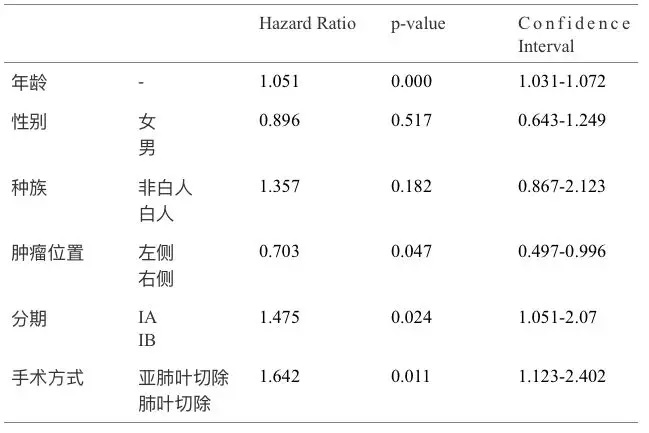
图. Cox比例风险模型
结论
在这项基于临床人群的研究中,肺叶切除术仍然是I期LCNEC患者手术的金标准,当技术和医学上可行时应作为首选。对于70岁以上无显著预后差异的患者,亚肺叶切除术可被认为是一种替代选择。
推荐阅读
文章评论
注册或登后即可发表评论
登录/注册
全部评论(0)