2019-04-12
作者:广东省肺癌研究所 杨学宁 & LAMP
新辅助免疫治疗后的肺切除术:并发症和微创治疗
22. Pulmonary Resection After Neoadjuvant Immunotherapy: Morbidity, Morality, and Use of Minimally Invasive Approaches
*Brendon M. Stiles, *Jeffrey L. Port, Benjamin Lee, Sebron Harrison, Mostafa Naguib, Mohamed Kamel, *Nasser K. Altorki
Weill Cornell Medical Center, New York, NY
Invited Discussant: *Chadrick E. Denlinger
Objective: Neoadjuvant immunotherapy (nIO) trials for early stage non-small cell lung cancer (NSCLC) are increasingly prevalent following favorable outcomes associated with immune-check point inhibitors in advanced disease. Early experience suggests that surgical resection after nIO may pose unique challenges unlike those experienced after neo-adjuvant cytotoxic therapy. We sought to compare the surgical approach and perioperative outcomes of patients receiving nIO with that of patients undergoing neoadjuvant chemotherapy (nCT).
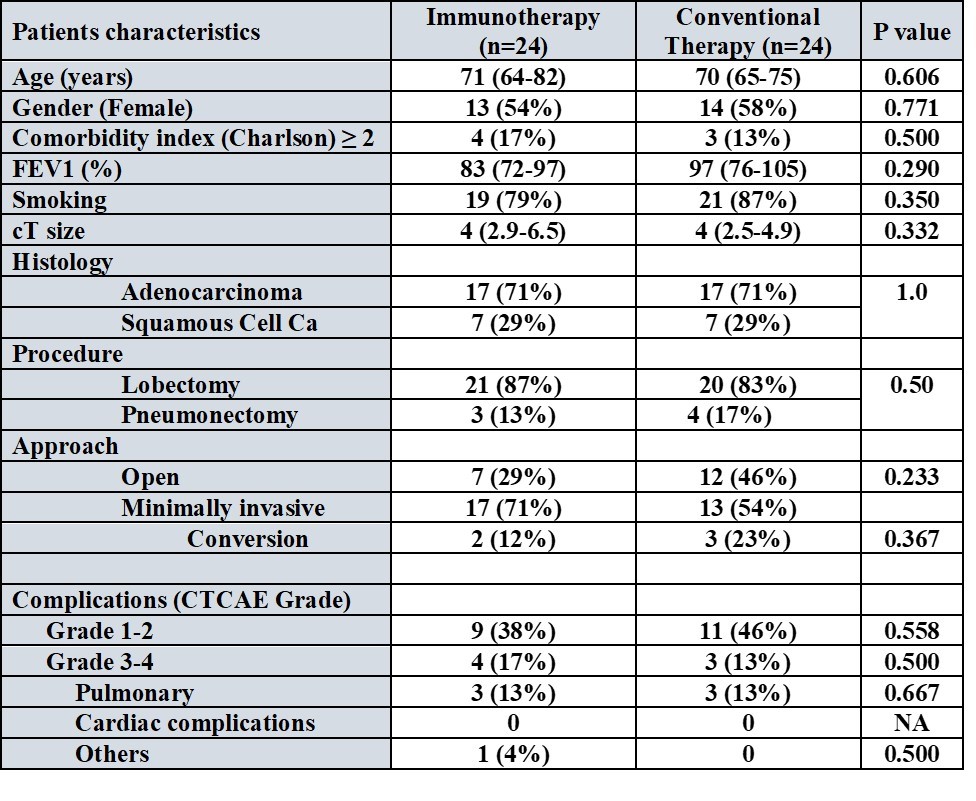
Methods: We identified 24 NSCLC patients who underwent an anatomic resection after nIO. Among these, 22 patients were part of an investigator initiated trial (NCT02904954) of neoadjuvant durvalumab, while 2 patients had received pembrolizumab+chemotherap prior to resection. From our prospectively maintained database, we propensity matched (1:1, Caliper 0.2: age, gender, smoking history, comorbidities, resection type) these patients to 24 patients undergoing nCT. Comparisons between groups were performed using Mann-Whitney U, Fischer’s Exact or Chi (X2) tests. The Common Terminology Criteria for Adverse Events (CTCAE) was used to grade postoperative complications.
Results: Median cT size was 4 cm (IQR 2.9-6.5 cm) in the nIO group and 4 cm (IQR 2.5-4.9 cm) in the nCT group (p=0.33). Lobectomy was performed in 87% of the nIO and 83% of the nCT groups respectively (p=0.50), while the remaining patients underwent pneumonectomy. More nIO patients underwent complete minimally invasive resections (63% vs. 42%, p=0.012), with less median blood loss (100cc vs. 150cc, p=0.05), and no statistical difference in operative time (172 minutes vs. 212 minutes, p=0.32). The conversion rate from minimally invasive to open was similar in the groups (12% for nIO vs. 23% for nCT, p=0.37). Only one intraoperative complication occurred in each group (nIO: airway injury; nCT: pulmonary artery injury). Between nIO and nCT groups there were no differences in the rate of any CTCAE Grade 3-4 total complications (17% vs. 13%, p=0.50), pulmonary complications (13% for each, p=0.67), cardiac complications (0 for both), or 30-day mortality (0 vs. 0). Median length of hospital stay was identical between nIO and nCT patients (5 days vs. 5 days, p=0.96).
Conclusions: Surgical resection after nIO is not associated with increased morbidity or mortality compared to that after neoadjuvant chemotherapy. Most resections can be accomplished minimally invasively.
推荐阅读
文章评论
注册或登后即可发表评论
登录/注册
全部评论(0)