2019-04-12
作者:广东省肺癌研究所 杨学宁 & LAMP
316. Surgery Is Associated with Survival Benefit in Select Patients with Clinical N3 Non-Small Cell Lung Cancer
Vignesh Raman1, Oliver K. Jawitz1, Paul J. Speicher1, Chi-Fu J. Yang2, *Thomas A. D'Amico1, Jacob Klapper1, *Matthew G. Hartwig1, *David H. Harpole1, *Betty C. Tong1
1Duke University, Durham, NC; 2Stanford University, Palo Alto, CA
Invited Discussant: *Lijie Tan
Objective: The National Comprehensive Cancer Network (NCCN) guidelines recommend definitive chemoradiotherapy alone for clinical N3 non-small cell lung cancer (NSCLC). However, the role of surgery in clinical N3 disease is not well described. We examined the outcomes of surgery for patient with cN3 NSCLC in the National Cancer Database (NCDB).
Methods: The NCDB was used to identify adult patients with cT1-3N3M0 NSCLC from 2004-2015. Patients with no treatment, incomplete definitive therapy, and missing staging or treatment information were excluded. Patients were stratified by treatment: definitive chemoradiation (CR) or surgery with or without chemoradiation (S). Overall survival was analyzed using Kaplan Meier and Cox proportional hazards models.
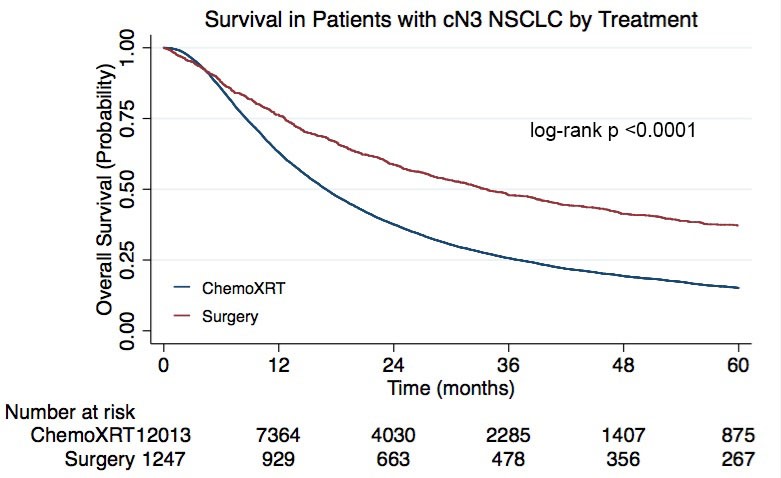
Results: A total of 14,918 patients met study criteria, of whom 13,548 (91%) were treated with definitive therapy and 1370 (9%) with surgery. Compared to CR patients, S patients were more likely to have a higher Charleson-Deyo Comorbidity Index (CDCC) score (43% >0 vs. 34%; p<0.001), be treated at an academic institution (38% vs. 30%; p<0.001), and have a lower clinical T stage (mean tumor size 33 vs. 38 cm; p<0.0001). Lobectomy (n=684; 66%) and wedge resection (n=229; 22%) were the most common operations. The median survival for CR and S patients was 17 (95% confidence interval [CI] 16,17) and 34 (95%CI 30,38) months, respectively. Surgery was associated with a significant survival benefit compared to definitive therapy in both univariable (p<0.0001; Figure 1) and multivariable analyses (hazard ratio [HR] 0.55; 95%CI 0.51,0.60). Lobectomy was associated with improved survival compared to wedge resection (HR 0.60; 95%CI 0.46,0.78). In the surgery group, 170 (12%) patients underwent neoadjuvant chemoradiation, 96 (7%) neoadjuvant chemotherapy alone, 483 (35%) adjuvant chemotherapy, 290 (21%) adjuvant chemoradiation, and 452 (33%) no perioperative therapy. Neither the receipt of neoadjuvant therapy (HR 0.85; 95%CI 0.67,1.07) nor adjuvant therapy (HR 0.85; 95%CI 0.69,1.04) independently predicted survival. Eighty percent of S patients (n=729) had pathologic nodal downstaging, including 49% (n=448) with pN0 disease. In a subgroup analysis of patients in both CR (n=1157) and S (n=187) groups with clinical and pathologic N3 disease, surgery independently predicted survival compared to chemoradiation (HR 0.77; 95%CI 0.63,0.95).
Conclusions: In this analysis, surgery was associated with a survival benefit compared to definitive therapy in a cohort of patients with clinical N3 disease and a high rate of pathologic nodal downstaging. Surgery may provide a survival benefit compared to definitive chemoradiation in carefully selected patients with clinical N3 NSCLC.
目的
NCCN指南建议单独使用根治性放化疗治疗临床N3 NSCLC。然而,手术在临床N3 NSCLC中的作用尚未得到很好的研究。我们评估国家癌症数据库(NCDB,National Cancer Database)中cN3 NSCLC患者接受手术治疗的效果。
方法
使用2004~2015年NCDB统计的cT1-3N3M0 NSCLC成人患者。没有治疗、非根治性治疗、缺失分期或治疗信息的患者被排除在外。基于治疗方法对患者进行分组:根治性放化疗组(CR)以及有或没有放化疗的手术治疗组(S)。使用Kaplan Meier和Cox比例风险模型分析总体存活率。
结果
共有14 918名患者符合研究标准,其中13 548名(91%)接受根治性性放化疗治疗,1 370名(9%)接受手术治疗。与CR患者相比,S患者更有可能获得更高的Charleson-Deyo合并症指数(CDCC)评分(43%>0 vs. 34%;P<0.001),在学术机构接受治疗(38% vs. 30%;P<0.001),并且具有较低的临床T分期(平均肿瘤大小33 cm vs. 38 cm;P<0.0001)。肺叶切除术(n=684;66%)和楔形切除术(n=229;22%)是最常见的手术。CR和S患者的中位生存期分别为17(95%CI 16,17)和34(95%CI 30,38)个月。与CR组相比,手术治疗在单因素(P<0.0001;图2)和多因素分析(HR 0.55;95%CI 0.51,0.60)中都能让患者获得显著的生存受益。与楔形切除相比,肺叶切除术与改善的生存率相关(HR 0.60;95%CI 0.46,0.78)。在手术组中,170例(12%)患者接受新辅助放化疗、96例(7%)单纯新辅助化疗、483例(35%)辅助化疗、290例(21%)辅助放化疗、452例(33%)无围手术期治疗。接受新辅助治疗(HR 0.85;95%CI 0.67,1.07)和辅助治疗(HR 0.85;95%CI 0.69,1.04)均无法独立预测生存率。80%的S患者(n=729)有病理性淋巴结降期,其中包括49%(n=448)的pN0患者。在患有临床和病理性N3疾病的CR(n=1157)和S(n=187)组患者的亚组分析中,手术相比放化疗能够独立预测存活率(HR 0.77;95%CI 0.63,0.95)。
结论
在该分析中,具有临床N3 NSCLC和高概率病理性淋巴结降期的患者中,与根治性治疗相比,手术治疗能够带来生存获益。在细心选择的临床N3 NSCLC患者中,与根治性放化疗相比,手术可提供生存获益。
图2. cN3 NSCLC患者治疗后的生存率
推荐阅读
文章评论
注册或登后即可发表评论
登录/注册
全部评论(0)